Auditory health can affect an individual’s quality of life and impact more than their hearing ability. It is important to take care of your hearing as you would any other aspect of your health, and audiologists play a vital role in this. Audiologists are healthcare professionals specialized in the diagnosis and treatment of hearing and balance disorders. They work to evaluate, diagnose, and treat patients of all ages, from newborns to the elderly. In this article, we will take a closer look at the role audiologists play in healthcare, the range of patients and concerns they treat, and the path to becoming a hearing healthcare professional.
Audiologists are doctoral-level hearing healthcare professionals who diagnose, evaluate and treat hearing loss as well as balance disorders. Responsible for educating patients on their hearing health, audiologists help protect their patients’ hearing and recommend and fit the assistive device most appropriate for them. Beyond this, audiologists also research hearing loss, tinnitus and balance disorders. Hearing health is important for a variety of factors and effects more than just auditory function. Proper ear care and protection is essential to preserve your hearing, whether you have mild hearing loss or more profound. However, your ability to hear can also impact other areas of your physical and emotional health. Our hearing ability plays a large role in facilitating communication, and trouble hearing can make this more difficult or even lead individuals to avoid socializing or isolate themselves. Caring for your hearing and managing hearing loss has also been shown to help support cognitive health and brain function. Taking care of your auditory health regularly can go a long way in supporting overall wellness and your quality of life.
Audiologists conduct hearing tests in a sound-treated room to ensure accurate results. There are several different types of hearing tests, and the audiologist will select the most appropriate test based on the patient's age, symptoms and medical history. Before beginning a hearing test, the audiologist will start by asking the patient about their medical history, any hearing difficulties they are experiencing, and any other relevant information. During the exam, they will use a tool called an otoscope to examine the patient's outer ear and ear canal for any signs of earwax buildup, infection, or other issues that could affect the hearing test results.
There are four different types of hearing tests an audiologist may conduct: pure-tone audiometry, speech audiometry, middle ear tests and otoacoustic emissions tests. Pure-tone audiometry tests are the most common diagnostic test done and are used to measure hearing sensitivity by assessing the softest sound a patient can hear. A speech audiometry test assesses the patient's ability to hear and understand speech. Speech audiometry consists of two tests; one test checks how loud speech needs to be for the patient to hear it while the other checks how clearly they can understand different words during speech. Middle ear tests assess the function of the middle ear, including the eardrum and the three small bones, known as ossicles, that transmit sound.

The audiologist may perform a tympanometry test which measures how the eardrum moves and indicates how well the middle ear is working. Testing of the middle ear is especially important for young children and can help indicate ear infections and other ear issues. Otoacoustic emissions tests (OAE) are used to evaluate how the cochlea in the inner ear is functioning. This test measures the sounds produced by the inner ear in response to a sound stimulus. The patient wears headphones or earplugs, and a small probe is placed in the ear canal to measure the OAE.
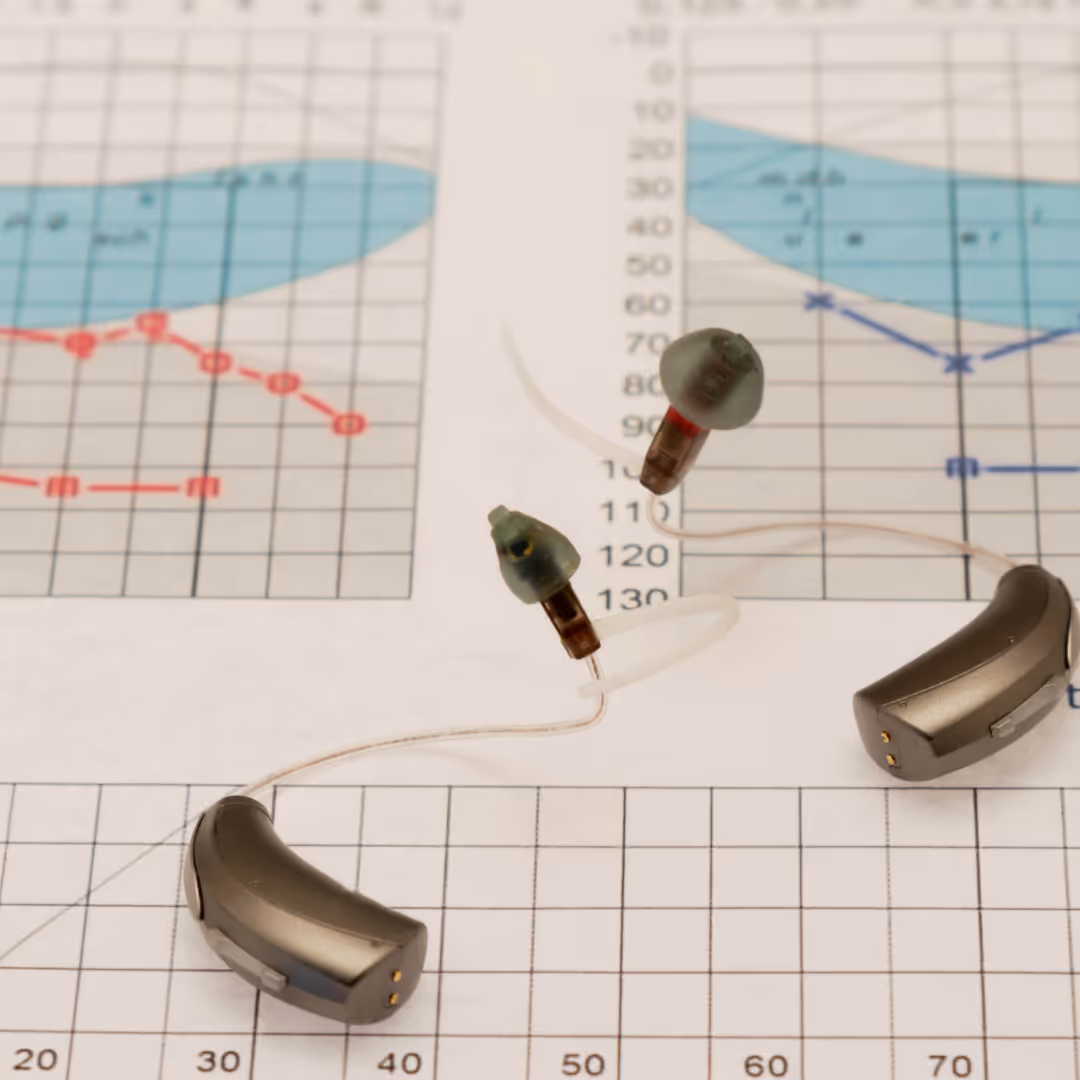
After conducting the hearing test, the audiologist will review the results to determine the patient's degree and type of hearing loss. An individual's hearing sensitivity is then plotted on an audiogram, which is a graph or chart showing how well one hears in terms of frequency.This shows the patient's hearing thresholds across different frequencies and decibel levels. The audiologist will use the audiogram to determine the type of hearing loss the patient has, such as conductive, sensorineural, or mixed hearing loss, and the degree of hearing loss, such as mild, moderate, severe, or profound. Based on the hearing test results and the patient's specific needs and lifestyle, the audiologist may recommend various assistive devices, such as hearing aids, cochlear implants, or other hearing devices, to help the patient hear better. The audiologist will typically work closely with the patient to select the appropriate device and provide ongoing support and follow-up care to ensure the device is working effectively.
In order to interpret the results of a hearing test, the audiologist will look at several factors. Factors considered include the patient’s hearing thresholds, type and degree of hearing loss, and the configuration of the hearing loss. A patient’s degree of hearing loss refers to the severity of the hearing disorder and may be classified as mild, moderate, severe, or profound. Configuration of the hearing loss refers to the pattern of hearing loss across different frequencies. Normal hearing is typically defined as the ability to hear sounds between 0-20 decibels (dB) at all frequencies tested. If the patient's hearing thresholds are outside the normal range, this indicates that the patient has a hearing disorder. The type of hearing loss indicates which part of the ear or auditory system is affected. Conductive hearing loss occurs when sound is not conducted properly through the outer and middle ear. Sensorineural hearing loss occurs when there is damage to the inner ear or auditory nerve. Mixed hearing loss is a combination of both conductive and sensorineural hearing loss. By analyzing all of these factors together, the audiologist can not only diagnose the type and degree of hearing loss, but make informed treatment options and recommendations.
Vestibular disorders affect the inner ear, or vestibular system, which is responsible for providing the brain with information about the body's position and movement in space. When diagnosing vestibular disorders, audiologists typically use a variety of tests to assess the patient's balance, coordination, and eye movements. These tests may include videonystagmography (VNG), rotary chair testing, posturography, and other specialized tests. Vertigo, vestibular neuritis and Meniere’s disease are a few examples of vestibular conditions. Once a vestibular disorder is diagnosed, the audiologist may recommend a variety of treatments, including medication, vestibular rehabilitation exercises, and lifestyle modifications to help manage symptoms and improve the patient's quality of life.
Audiologists offer a range of treatment services for individuals with hearing and balance disorders. These services may include hearing evaluations, where audiologists assess hearing ability and diagnose hearing loss. They may also provide hearing aid and cochlear implant evaluations, which involve selecting and programming hearing devices to improve hearing function. Audiologists also offer balance assessments and vestibular rehabilitation, which can include specialized exercises to improve balance and coordination. They may provide tinnitus evaluations and treatment, offering sound therapy or other management strategies to reduce the impact of tinnitus symptoms. Additionally, audiologists may offer counseling and education to individuals and their families on how to cope with hearing and balance disorders and adapt to changes in their daily lives. Overall, audiologists provide a comprehensive range of services to help individuals with hearing and balance disorders achieve improved function and quality of life.
Hearing assistive devices are not the end all be all for sensory loss, despite today’s technological advancements. In order to maximize the benefits of hearing aids and other assistive technology, wearers should also utilize auditory training. An estimated 40% of dispensed devices may not be used effectively or at all. Auditory training, sometimes referred to as aural rehabilitation, aims to enhance the use and satisfaction of hearing aids and cochlear implants. These hearing assistive devices can help to amplify sound, but they do not necessarily restore normal hearing, and individuals may still struggle with understanding speech or distinguishing between different sounds. Through auditory training, individuals can practice and improve their ability to perceive and process sounds in a way that is more natural and effective.
This can include exercises designed to help individuals identify and discriminate between different speech sounds, as well as strategies for improving listening skills in different environments. By improving their auditory processing abilities, individuals with hearing aids or cochlear implants can often see significant improvements in their ability to communicate and engage with the world around them.
Audiologists play a critical role in determining the most appropriate hearing aids for a patient based on their specific hearing needs, preferences, and lifestyle. They also provide guidance on how to properly use and care for hearing aids, as well as how to adjust to wearing them. In addition, audiologists can program and adjust hearing aids to ensure they are working optimally, and provide ongoing support.
Similarly, audiologists are also key in supporting their patients who have or could benefit from cochlear implants. They are involved in the selection, programming, and management of cochlear implant devices for individuals with severe to profound hearing loss who are not able to benefit from traditional hearing aids. Audiologists work with individuals and their families to assess whether a cochlear implant is a suitable option and provide guidance throughout the process. They program and fine-tune the implant to ensure optimal performance and provide ongoing support, including counseling and training, to help individuals adapt to their new hearing capabilities. For those who are candidates for cochlear implants, audiologists also work closely with other healthcare professionals, such as surgeons and ear nose and throat doctors (ENT), to ensure comprehensive care.
Patients who have vestibular issues can also receive council and services from an audiologist. They are trained to assess and diagnose vestibular disorders and provide guidance on appropriate treatment options. Treatment plans may include specialized exercises to improve balance, coordination, and overall function of the vestibular system. Aside from rehabilitation, audiologists may also provide support to patients, including counseling and education on how to adapt to changes in balance and mobility.
In order to become an audiologist, prospective candidates must complete their doctoral degree, complete a fellowship program or externship and pass licensing exams. As of 2007, a doctorate in audiology, or AuD, became the entry-level degree for the clinical practice of audiology. However, professionals who completed their masters degree in audiology prior to 2007 are not required to have a doctorate. Prior to receiving an AuD, students typically receive their undergraduate degree in speech and hearing science. Bear in mind that different audiology programs may accept students with undergraduate backgrounds in other disciplines or areas of science, given that they have completed the necessary prerequisites.
In general, a master's degree in audiology may take two to three years of full-time study to complete. However, some programs may offer an accelerated option that allows students to complete the program in a shorter period. It is important to note that a Doctor of Audiology (Au.D.) degree is necessary to meet licensure requirements. While a master’s degree is not required, some students may choose to complete a Master’s of Science in speech pathology or a related field as these skill sets may be beneficial when working with patients with profound hearing loss.
The Au.D. degree is a four-year, post-bachelor's degree program that includes both coursework and supervised clinical experiences. It prepares students to work as audiologists and to provide diagnostic, rehabilitation, and other services related to hearing and balance disorders. Foundational coursework is covered in the first two years of an AuD program, and the third and fourth year consist of hands-on experience through clinical hours and externships. An audiology externship is a supervised clinical experience that allows audiology students to gain hands-on experience in the field of audiology. During an audiology externship, students work under the supervision of licensed and experienced audiologists in a clinical setting, such as a hospital, audiology clinic or private practice. This experience allows students to apply the knowledge and skills they have learned in the classroom to real-world situations and to gain experience working with patients of all ages and with a variety of hearing and balance disorders. Externships expose students to a wide range of necessary skill sets including: conducting hearing tests, developing treatment plans, fitting and dispensing hearing aids and other assistive devices, as well as counseling patients and family members on hearing conservation and communication strategies.
After completing the Au.D. degree, graduates must typically pass a national examination and obtain state licensure to practice as audiologists. Graduates must first pass the Praxis Examination in Audiology as a requirement for certification and state licensure. Requirements for licensure vary by state, and each state also determines what score on the Praxis Exam is required. It is recommended to research the requirements for the specific state or country where you plan to practice audiology. Additionally, state requirements may include passing a state-specific exam, completing continuing education courses, and meeting other requirements related to professional ethics and conduct. National certification for audiologists in the United States is governed by two organizations, the American Speech-Language-Hearing Association (ASHA) and the American Board of Audiology.
Continuing education credits are required to maintain audiology licensure and certifications, in an effort to help professionals stay up to date on technology and best practices. The amount of continuing education units (CEUs) that are needed depends on whether or not the audiologists are also responsible for dispensing hearing aids and assistive devices or not. Non-dispensing audiologists must complete 24 hours of continuing education each license renewal period, every two years. Dispensing audiologists have to undergo 12 hours of continuing education units each year. For both dispensing and non-dispensing audiologists, licenses expire on the date of issuance, either one or two years, respectively, after issuance. All qualifying CEUs must first be approved by the American Academy of Audiology. Courses are approved based solely on content, with the goal being to ensure quality of education and that professionals obtain a full range of training.
Audiologists may choose to specialize in various areas of audiology based on their interests and career goals. Some common areas of specialization in audiology include: pediatric, geriatric, educational and industrial audiology along with tinnitus and vestibular disorders. Some audiologists may also choose to work primarily in research or as professors, or choose to specialize in other areas like auditory processing disorders. They may also focus professionally in the area of hearing assistive devices like hearing aids and cochlear implants, recommending and fitting patients with the assistive technology to best meet their individual accessibility needs and improve quality of life.

Pediatric audiologists work with children, infants, and newborns to diagnose and treat hearing and balance disorders. They may also work with children who have speech and language delays related to their hearing loss. Geriatric AudiologistsGeriatric audiologists work with older adults to diagnose and treat age-related hearing loss and balance disorders. Those serving the senior population sometimes also work with patients who have other age-related conditions that can affect hearing, such as dementia.
Balance and vestibular audiologists specialize in the diagnosis and treatment of balance disorders and dizziness. These audiologists often work alongside patients who have conditions such as vertigo, Meniere's disease, or vestibular neuritis.
Professionals who focus on treating patients with tinnitus, a buzzing or ringing sensation in the ears, provide counseling and therapy to help patients manage their symptoms. Industrial audiologists work in occupational health and safety to protect workers from noise-induced hearing loss and other hearing-related conditions. They may provide hearing protection devices, conduct hearing screenings, and assess workplace noise levels.
Educational audiologists deliver hearing services to children in an educational setting. They facilitate learning, listening and communication skills through specialized assessments in addition to recommending, fitting and monitoring hearing assistive devices for students who need them. Additionally, they counsel students on self-advocacy and may collaborate with private-sector audiologists and other school professionals.
Audiologists work with a variety of healthcare professionals to provide comprehensive care to patients with hearing and balance disorders. Some of the healthcare professionals that audiologists may work with include ENTs, speech language pathologists and occupational therapists. Through working alongside such healthcare professionals, audiologists help treat a wide array of individuals with hearing loss or disorders affecting their lives in different aspects.

Ear, nose, and throat (ENT) doctors and audiologists often work together in the diagnosis and treatment of ear-related conditions. ENT physicians specialize in the medical and surgical management of conditions affecting the ears, nose, and throat, while audiologists focus on the assessment and treatment of hearing and balance disorders. When a patient presents with hearing loss, tinnitus or balance problems, an ENT doctor will typically refer the patient to an audiologist for a comprehensive hearing evaluation. The audiologist will perform tests to assess the patient's hearing and balance function, and will work with the ENT doctor to determine the underlying cause of the patient's symptoms. Based on the results of the evaluation, the ENT doctor and audiologist will work together to develop a personalized treatment plan that may include medication, surgery, or the use of hearing aids or other assistive listening devices. By collaborating, ENT doctors and audiologists can provide patients with the most effective and appropriate care for their specific ear-related conditions.
Speech pathologists focus on diagnosing and treating communication and swallowing disorders. In cases where hearing loss is impacting speech and language development, audiologists and speech pathologists will collaborate to create a comprehensive treatment plan that addresses both the hearing and communication issues. Audiologists may provide hearing aids or cochlear implants to improve hearing, while speech pathologists may develop personalized therapy plans to help patients improve their speech and language abilities. By working together, audiologists and speech pathologists can provide patients with the most effective and individualized care possible.
Occupational therapists (OTs) and audiologists may work together in cases where a patient's hearing loss is impacting their ability to perform daily activities. OTs are healthcare professionals who specialize in helping individuals develop or recover skills needed for daily living and work. When a patient is experiencing difficulty in communicating or participating in activities due to their hearing loss, an OT may refer the patient to an audiologist for a hearing evaluation. The audiologist will then work with the OT to determine the specific challenges the patient is facing and develop a personalized treatment plan to improve their ability to communicate and participate in daily activities. This may include recommending hearing aids or other assistive listening devices, as well as providing education and counseling to help the patient adapt to their hearing loss.
Early diagnosis of hearing disorders or hearing loss is critical to improving outcomes and preventing further complications. Hearing plays a critical role in communication, speech, language and social development, making early detection and intervention essential for infants, children and adults. Untreated hearing loss can lead to delayed language and speech development, social isolation and cognitive decline, among other issues. Additionally, it can have an impact on academic performance, employment opportunities, and overall quality of life. Early identification of hearing loss allows for prompt treatment, which can include the use of hearing aids, cochlear implants or other assistive devices, as well as speech therapy and other interventions. By detecting hearing loss early, individuals can receive the appropriate care and support needed to minimize the impact of hearing loss and maximize their communication abilities, leading to improved outcomes and quality of life.
Audiologists use hearing test results to help prevent further damage in patients with hearing loss by identifying the extent and type of hearing loss, as well as the underlying cause. Based on the results of the hearing tests, the audiologist can develop a personalized treatment plan, which may include the use of hearing aids or other assistive devices, as well as education and counseling on how to prevent further hearing loss. For example, if the hearing loss is due to exposure to loud noise, the audiologist may advise the patient on how to protect their ears from loud noises, such as using earplugs or avoiding noisy environments. Additionally, the audiologist may work with the patient to develop communication strategies that can help them to better understand speech and navigate difficult listening environments. By using hearing test results to develop a personalized treatment plan, audiologists can help patients with hearing loss to manage their condition and prevent further damage, leading to improved communication abilities and overall quality of life.
Hearing tests can help audiologists discover underlying health issues by providing insight into the functioning of the auditory system. This can help identify conditions that may be contributing to hearing loss, such as Meniere's disease, autoimmune disorders, ear infection or neurological concerns. For example, if a patient's hearing test results indicate that they have difficulty understanding speech in noisy environments, this may suggest that they have a condition affecting the auditory nerve, such as multiple sclerosis. Similarly, if a patient's hearing test results indicate sudden or fluctuating hearing loss, this may suggest the presence of an autoimmune disorder. By identifying these issues through hearing tests, audiologists can refer patients to the appropriate medical professionals for further evaluation and treatment. In some cases, early detection and treatment of underlying health issues can help prevent further complications and improve overall health outcomes. Overall, understanding hearing test results is crucial for early detection, accurate diagnosis, and appropriate intervention, which can improve outcomes and quality of life for people with hearing loss.
The appropriate treatment option for hearing loss and hearing disorders will depend on the type and degree of hearing loss, as well as individual needs and preferences. An audiologist can help determine the most appropriate treatment option based on a comprehensive hearing evaluation. There are several treatment options for hearing loss and hearing disorders, including hearing aids and assistive devices, cochlear implants and auditory training. For patients who have tinnitus or vestibular disorders, audiologists can also assist with symptom management and customized treatment plans.
Hearing aids and other assistive devices are commonly used as a treatment for hearing loss. These devices work by amplifying sound and improving speech clarity, making it easier for patients with hearing loss to communicate and engage in social activities. Hearing aids typically consist of a microphone, amplifier, and speaker, and can be custom-fitted to a patient's ear for optimal comfort and effectiveness. Other types of assistive devices may include personal amplifiers. Audiologists can help patients select the appropriate hearing aid or assistive device based on their degree and type of hearing loss, lifestyle, and communication needs.
Cochlear implants are a type of medical device used to treat hearing loss in individuals with severe-to-profound hearing loss who receive little benefit from hearing aids.

These devices consist of two parts: an internal component that is surgically implanted under the skin behind the ear, and an external component that sits on the outside of the ear and is connected to the internal component by a magnet. The internal component contains a tiny electrode array that is inserted into the cochlea, the spiral-shaped structure in the inner ear responsible for sending sound signals to the brain. The external component captures and processes sound signals, which are then transmitted to the internal component and delivered directly to the auditory nerve. Audiologists work closely with patients and their medical teams to evaluate candidacy for cochlear implants, conduct preoperative testing, and provide postoperative programming and rehabilitation to optimize the patient's use of the device.
Auditory training is a form of rehabilitation that involves specific exercises designed to help individuals with hearing loss or disorders improve their ability to understand speech and other sounds. This type of training can be particularly beneficial for people who use hearing aids or cochlear implants, as it can help them to better perceive and process sounds in a way that is more natural and effective. During auditory training, individuals may work with a speech-language pathologist or audiologist to practice identifying and discriminating between different sounds and speech patterns, as well as to learn strategies for improving their listening skills in different settings.
Tinnitus is a condition characterized by the perception of sound in the absence of an external sound source. While there is no cure for tinnitus, there are several treatment options and management strategies that can help individuals to reduce the impact of symptoms and improve their overall quality of life. One of the most common treatments for tinnitus is sound therapy, which involves the use of external sounds to mask or distract from the perceived tinnitus sounds. This can include white noise machines, music, or specialized devices that produce specific sounds tailored to an individual's tinnitus. Cognitive behavioral therapy (CBT) can also be effective in helping individuals to manage the emotional distress and negative thoughts that can accompany tinnitus. It is important for individuals with tinnitus to work closely with their healthcare provider to determine the best treatment approach for their specific needs and symptoms.
Vestibular rehabilitation is a specialized form of physical therapy that focuses on improving balance and reducing dizziness in individuals with vestibular disorders. Treatment options for vestibular rehabilitation may include exercises designed to improve the function of the vestibular system, such as gaze stabilization and balance retraining exercises. These exercises may involve movements of the head and body, as well as visual cues and other sensory input. Other treatment options may include canalith repositioning maneuvers, which are used to reposition displaced particles within the inner ear that can cause vertigo, and habituation exercises, which involve exposing individuals to specific movements or stimuli that trigger dizziness in order to help them adapt and reduce symptoms over time.
Audiologists can offer a range of communication strategies to their patients to help them better understand speech and navigate difficult listening environments. One common strategy is to emphasize the use of visual cues, such as lip-reading and facial expressions, to supplement auditory information. Audiologists may also recommend specific communication strategies, such as speaking in a quiet environment or facing the patient when speaking. Other communication strategies may include the use of speech therapy or other educational programs that teach patients how to effectively communicate in different settings. By offering these strategies for communication, audiologists can help their patients overcome the challenges of hearing loss and improve their ability to communicate with others, leading to improved social interactions, academic and work performance.
Hearing healthcare providers also offer their patients advice on coping skills to better adjust to their hearing loss emotionally. Audiologists may connect their patients with support groups and counseling to help them cope with the emotional and psychological impacts of hearing loss. Support groups can provide a supportive environment where patients can connect with others who have similar experiences and share coping strategies and tips. Counseling may be offered by a mental health professional who can help patients address emotional issues related to hearing loss, such as depression or anxiety. Additionally, audiologists may provide education and counseling to family members to help them better understand the impact of hearing loss on their loved ones and learn how to communicate more effectively with them. By connecting patients with support groups and counseling, audiologists can help patients manage the emotional and psychological impact of hearing loss and improve their overall well-being.
Hearing health is essential and hearing loss can have significant impacts on communication, socialization, employment opportunities, mental health and cognitive function. Conducting individualized treatment plans and recommending assistive hearing devices, audiologists improve their patients’ quality of life. They can also provide counseling and support for individuals with hearing loss and auditory disorders and work with other healthcare professionals to provide coordinated care. It is important to see an audiologist if you are experiencing any signs of hearing loss, such as difficulty understanding speech, ringing in the ears, or increased difficulty hearing in noisy environments. It is also recommended to have regular hearing evaluations, especially as you age or if you are at higher risk for hearing loss due to exposure to loud noises, certain medications, or underlying health conditions. Overall, taking care of your hearing health is crucial for overall well-being, and audiologists play an essential role in ensuring optimal hearing health.
An audiologist is a healthcare professional who specializes in the diagnosis and
treatment of hearing and balance disorders.
There are several ways to find a qualified audiologist including: referral from a healthcare provider, online directories or through your insurance company’s list of in-network providers. When choosing an audiologist, it's important to consider education and credentials, experience, and reviews from previous patients. It's also a good idea to schedule a consultation or appointment with the audiologist to ensure that you feel comfortable with them and their approach to care.
During a hearing test, you can expect to have your ears examined, listen to different tones and speech, and potentially undergo additional testing. The audiologist will review the results with you and recommend treatment options if necessary.
Ways to protect hearing include wearing earplugs or earmuffs in loud environments, taking breaks from loud noises, limiting exposure to loud noises, avoiding or minimizing the use of headphones or earbuds at high volumes, and maintaining a healthy lifestyle to reduce the risk of hearing loss associated with chronic diseases.
If you think you have a hearing problem, your first step should be to schedule an appointment with an audiologist for a hearing evaluation.
Tinnitus is a condition characterized by the perception of sound, such as ringing, buzzing, or hissing, in one or both ears. Although there is no known cure for tinnitus, your audiologist can help you manage the symptoms with different treatment plans. Treatment options may include sound therapy, cognitive behavioral therapy to help patients develop coping strategies, or the use of hearing aids or other assistive devices to improve hearing and reduce the perception of tinnitus.
Hearing aids are worn behind or in the ear and amplify sound and work by picking up sound from the environment and make it louder and clearer. A cochlear implant is a small electronic device that is surgically implanted into the inner ear to provide sound signals directly to the auditory nerve. It is typically recommended for individuals with severe to profound hearing loss who are not able to benefit from traditional hearing aids. Unlike hearing aids, cochlear implants do not amplify sound. Instead, they bypass the damaged portion of the inner ear and stimulate the auditory nerve directly to provide the perception of sound.
The time it takes to adjust to hearing aids varies for each individual, but it typically takes a few weeks to a few months to fully adapt to the new hearing experience provided by the hearing aids.
It is recommended that adults get their hearing tested at least once every 10 years up to the age of 50, and then every 3 years thereafter. However, if you are experiencing any changes in your hearing or have any concerns about your hearing, it is recommended that you see an audiologist as soon as possible.
Some insurance plans do cover hearing aids and audiology appointments, while others do not. It is important to check with your insurance provider to determine what is covered under your plan. Additionally, some insurance plans may have specific requirements for coverage, such as a referral from a primary care physician or a specific network of providers.
InnoCaption provides real-time captioning technology making phone calls easy and accessible for the deaf and hard of hearing community. Offered at no cost to individuals with hearing loss because we are certified by the FCC. InnoCaption is the only mobile app that offers real-time captioning of phone calls through live stenographers and automated speech recognition software. The choice is yours.